
There are many reasons for treating patients with medication, with the main three being:
Diagnosis – This is to investigate the cause of the illness or examine the nature of the symptoms.
Treatment – After the diagnosis, the medication is used to reduce symptoms and fight the illness.
Prevention – Medication to stop the illness or disease being developed.
What is administration of medication?
This is simply the route medication takes to enter your body. The medicine can come in many different forms and the method of administration differs depending on this, the illness and the patient’s needs.
Professional training is required for medication administration as even though its purpose is to improve our health, if done incorrectly, it can be highly dangerous.
Our nurse case managers receive regular expert training and are frequently checked against our high-level competencies for this reason.
The 6 routes of medication administration
When you think of taking medicine, you probably imagine swallowing a pill or receiving an injection. However, there are many ways to administer medication. The route we take for our patients depends on varying factors, such as the illness itself, the severity of the illness, the needs of the patient and their condition.
To get a better understanding, here are the 6 most common routes:
- Oral – Swallowed through the patients mouth as either a tablet, liquid, capsule, lozenge or chewable tablet.
- Rectal – This may be the next option for those who can’t swallow the medication. The drug is administered rectally as a suppository.
- Inhalation – Medication is inhaled through the patients airway in the form of a powder, aerosol spray or mist. This is most commonly used with a mask or tube, such as an inhaler.
- Nebulization – A nebulizer is a machine that allows the patient to inhale the drug as a very fine mist. This is similar to inhalation.
- Transdermal – This is a way to get the drug through the skin into the body without breaking the surface. A patch is placed on the patients skin with the medicine (sometimes mixed with a chemical) that penetrates into the blood stream.
- Injection – The four injection routes include intrathecal (into the spine), subcutaneous (under the skin), intravenous (into a vein) and intramuscular (into a muscle).
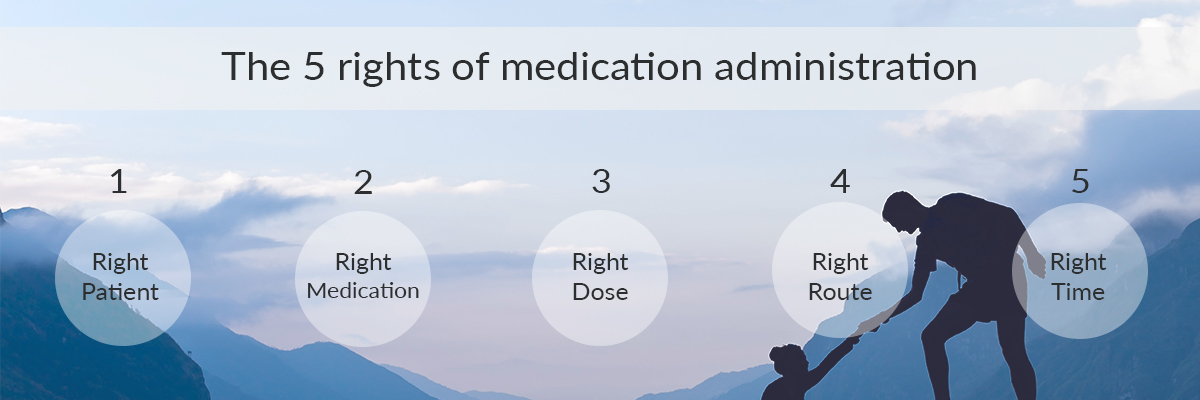
The 5 rights of medication administration
For safe medication administration, there is training, guidelines, competencies and good practice that we strictly follow at AJ Case Management.
To give you an idea of the safe practices we follow everyday with our patients, here are the 5 rights of medication administration:
- Right Patient – The patient must identify themselves, so the name can be checked on the order. Two or more identifiers should be provided.
- Right Medication – The prescription is thoroughly checked by reading the type of medicine it is and the expiry date to make sure this is correct.
- Right Dose – The dosage is assessed against the type of medication to confirm it is appropriate.
- Right Route – Using our own knowledge and the information on the label we assess whether the right route of administration has been recommended.
- Right Time – The frequency of the medication is checked so that we can confirm we are giving the patient their medicine at the right time.
Administration of Rescue Medication – Buccal Midazolam, GTN for Autonomic Dysreflexia
When we refer to rescue medication, we are talking about medicine that is administered to give immediate relief for the symptoms of the condition.
This quick-acting medicine is a short-term solution and temporarily reduces the symptoms you are suffering with.
What type of illnesses should rescue medication be used for?
Rescue medication can be used to treat a wide range of illnesses, ranging from mild severity to serious conditions. Here are the most common conditions that rescue medicine is used for:
Seizures – Some patient’s seizures may usually last the same amount of time and stop by themselves without the use of medication. However, some seizures may be more random and last a lot longer, without giving the patient time to recover in between.
This can be very dangerous and lead to status epilepticus. To prevent this, buccal midazolam is administered as it is a sedative. This has a calming effect on the brain which can stop the seizure.
Autonomic Dysreflexia – Also known as AD, this is a condition where your autonomic nervous system overreacts to a stimulus that occurs below the level of the injury.
It is most common in those with spinal cord injuries. AD can cause a spike in blood pressure or a rapid heartbeat.
GTN, also known as glyceryl trinitrate or nitroglycerin can be used as rescue medication to treat the heart problems associated with this condition.
Allergic reactions – allergies are very common and affect around 1 in 4 people in the UK. An allergy is your body reacting negatively to a particular food or substance. Symptoms caused by this condition could include:
- Itchiness
- Swelling
- Wheezing or trouble breathing
- Runny or blocked nose
- Irritated or watery eyes
- Swelling of the throat
There are many more symptoms you may experience which depend on the type of allergy and your level of exposure to the allergen.
Epinephrine is a rescue medication that can be administered in the form of injection to relax the muscles and calm your symptoms.
Asthma attacks – Although asthma is a common condition and for the majority the severity is mild, for some it can create a very dangerous situation where the patient’s life is at risk. Symptoms can include:
- Wheezing
- A feeling of tightness in your chest
- Coughing
- Breathlessness and difficulty breathing
Rescue medication for asthma attacks usually comes in the form of an inhalation drug.
Administration of Medication via PEG
Percutaneous endoscopic gastrostomy, also known as PEG, is where an external tube is inserted through a patient’s abdominal wall and into their stomach. This is mainly used for feeding and nutritional support, although it can also be used for the administration of medication.
This method is a long term solution and is usually not appropriate for short term requirements. It is ideal for patients who have trouble eating or swallowing.
What are the different types of PEG tubes?
There are many different types of PEG tubes that can be used for patients. The most common include:
PEG and long tubes – These types of tubes are usually used for the initial insertion. They are a single piece tube that are held in place by a bumper or retention balloon.
Low profile tubes or buttons – The long tube on the exterior of the body is not permanent and can be removed when the patient it not being fed or given medication. This is where the name comes from, as when the exterior tube is removed the button lays flat and is fairly unnoticeable.
What is the difference between a PEG tube and a J-Tube?
A jejunostomy feeding tube, also known as a J tube, is a feeding tube that is similar to a PEG tube. However, instead of the stomach, a J-Tube is inserted into the small intestine.
They are both required for similar reasons, usually for patients who have difficulty eating or swallowing.
A J-Tube may be required when a patient has an obstruction to the stomach. They are usually the preferred option over a PEG tube for a permanent solution.
For most patients a J-Tube can’t be changed at home and this procedure must be done by a professional. For a PEG tube, home changing is possible.
What training is required for administration of medication?
Training in administration of medication is essential for staff working in the health and social care sector. All of our staff who work with medication administration are fully trained in this field and receive regular refreshers and updates.
It is a common misconception that just nurses require this training, however this is not the case. Those who may require this kind of training could include:
- Nurses
- Social workers
- Full time/ part time carers
- Case managers
- Support workers
- Staff who work in a care home
Why is training in administration of medication needed?
Training in this field of care and nursing is ultimately for the safety and comfort of the patient. There are many things we can do to make sure we always put these things first with patients, some of which include:
- Identify and diligently follow the laws and legislations
- Understand and follow the rights of medication administration
- Recognise common medication and what it might be used for
- Understand and practice efficient record keeping
- Predetermine errors or dangers and create solutions to avoid them
- Understand the importance of confidentiality
Guidelines we follow to prevent errors in the administration of medication
The health and happiness of our patients is at the heart of everything we do at AJ Case Management. Our highly skilled team of professionals are continuously trained in rehabilitation and providing the best route to recovery.
A big part of this is establishing errors before they happen, which is a risk when administrating medication. Here are a few of the guidelines we follow to reduce this risk:
- Reminding ourselves of the 5 rights of medication administration and continuously following them.
- Providing the correct documentation and organising the information efficiently so it can be easily accessed and clearly understood when needed.
- Ensuring the correct storage of varying medications, such as keeping them refrigerated and making sure they are in the correct departments.
- Regular training to be aware of any updates in the medication sector.
- Ensuring patients are full aware of the medication they’re taking and what affect it will have on them.
- Ensure staff involved are educated on the necessary needs and requirements of the patient.
- Keep a record of past and current medications to ensure no conflict between medicines.
Recent Comments